Trauma to the eye is a preventable cause of
ocular injury. It is one of the leading causes of ocular morbidity1,2,3.
A large number of hospital visits are due to eye injury4. Superficial
ocular surface foreign body injury is the most common form of ocular trauma. It
causes significant discomfort and if not properly managed can lead to permanent
visual impairment. A patient may encounter this type of injury in a variety of
settings for example at home, while playing, at work or as a result of accident
orassault5.
Usually ocular surface foreign bodies are
small in size6. They are particles of iron, dust, insect wings,
straw of vegetable matter, animal or human hair and threads of cotton or
plastic. In most of the cases ocular surface foreign bodies are found on cornea
and palpebral conjunctival surfaces. They may also be found in fornices, sub
tarsal space and caruncle. Patients experience pain, foreign body sensation,
watering and redness. If left untreated and not properly managed they can lead
to erosion of underlying surface, establishment of infection, spread of infection
leading to infective keratitis, conjunctivitis and endophthalmitis7.
Thorough eye examination
including upper lid eversion is necessary in patients with history of foreign
body. Insects recovered from the eyes need to be examined by entomologist to identify
its nature, species and toxic effects if any. This may help in planning proper
and targeted spray to seasonal crops to decrease the number of insects. This is
useful in rural and semi-urban areas in term of economics, by reducing damage
to the crops. Identification of the type
of foreign bodies and their location of impaction into the eye will help in creating
awareness and use of appropriate eye protective devices. This study was done to
find the causes of ocular surface foreign bodies in a rural setting.
MATERIAL AND METHODS
This prospective study was conducted in Ophthalmology
department of Shahida Islam Medical College Lodhran. Duration of the study was
from November 2016 to October 2017. The study was approved by the ethical
committee of the institution. Consent was obtained from all patients who were
included in the study. All patients coming in eye outpatient department with foreign
body in eye were included in the study. This was a cross sectional study and
sampling technique was purposive sampling.
Age and gender were recorded for all
patients. Detailed slit lamp examination was performed. Fluorescein dye was
instilled in the eye to delineate the location of the foreign body. Topical anaesthesia
was given by instilling proparacaine 0.5%. Superficial foreign bodies were
removed with the help of forceps. In case of impaction, the ocular surface
foreign bodies were removed with the help of sterile 27/26 gauge needle. After
removal of the foreign body topical antibiotic drops was instilled into the
eye. Postoperatively topical antibiotic eye drops were prescribed for seven
days. Statistical analysis was performed using statistical programme for social
sciences (SPSS version 21).
Nominal variables like
gender, type and location of foreign body were presented as percentages.
Continuous variable like age was presented as mean and standard deviation.
Correlation of the type of foreign body with their location in the eye was
calculated using Pearson’s R correlation.
RESULTS
Total of 796 patients
with ocular foreign bodies were included in the study. On average 2.18 patients
with ocular surface foreign bodies presented per day. There were 378 (47.5%)
right eyes and 411 (51.6%) left eyes. There were 7 (0.9%) bilateral cases.
There were 568 (71.4%) males and 228 (28.6%) females. Male to female ratio was
2.5:1. Frequency and percentages of the type of foreign body are shown in table
1.
Table 1: Aetiology of ocular surface
foreign bodies.
|
Type of Foreign Body |
Frequency |
Percent |
|
Insect wing |
204 |
25.6 |
|
Metallic ring |
216 |
27.1 |
|
Straw particle |
156 |
19.6 |
|
Plastic |
48 |
6.0 |
|
Insect/fly |
24 |
3.0 |
|
Thread/cloth particle |
34 |
4.3 |
|
Dust particles |
112 |
14.1 |
|
Contact lens |
2 |
0.3 |
|
Total |
796 |
100.0 |
Frequency and percentage of location of
foreign bodies is shown in table 2. Frequencies of location of at Different
locations of foreign bodies in the eye are shown is table 2. Mean age of
patients was 38.58 ± 21.49 years and the mode age was 45 years.
The correlation between the
aetiology of foreign body and their location in the eye was found to be 0.088
(Pearson’s R correlation; Chi-square test). Correlation line between aetiology
of ocular surface foreign body and location in the eye is shown in figure 1. Results
showed there was no statistically significant correlation between the aetiology
of ocular surface foreign body and its location in the eye. Pictures of
different foreign bodies seen in the study are shown in figures 2-4.
Table 2: Distribution of location of
foreign bodie
|
Location of Foreign Body |
Frequency |
Percent |
|
Corneal |
320 |
40.2 |
|
Palpebral conjunctival |
147 |
18.5 |
|
Upper lid sub tarsal |
222 |
27.9 |
|
Inferior fornix |
51 |
6.4 |
|
Superior fornix |
14 |
1.8 |
|
Caruncle |
42 |
5.3 |
|
Total |
796 |
100.0 |
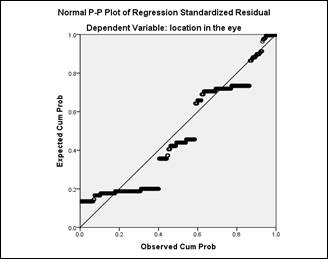
Figure 1: Regression line for aetiology
of ocular surface foreign body and their location in eye.
Key:
X axis = Type of foreign
body.
Y axis = Location in the
eye.
DISCUSSION
On an average 2.18
patients with ocular surface foreign bodies presented per day. Ocular injury
with ocular surface foreign bodies was more common in males than females. Male
to female ratio was 2.5:1. This is in close approximation to that presented by
Reddy et al8. Males are at greater risk
to trauma due to their exposure in occupation, travelling and assaults9.
Mean age in our study was 38.58 ± 21.49 years. Jahangir T and co-authors
reported mean age of 28.6 ± 17.6 years10. In another study the mean
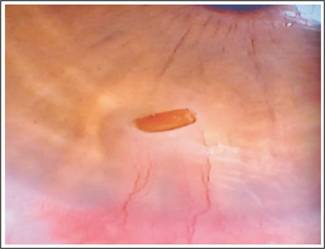
Figure 2:
Straw Particle at Cornea.

Figure 3:
Insect in Inferior Fornix.
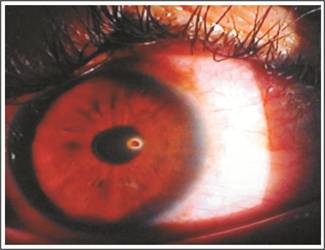
Figure 4:
Metallic Particle at Cornea.
age of
the patients was reported to be 35 years.
In 40.2% cases cornea was involved, in
18.5% cases palpebral conjunctiva, in 27.9% cases upper lid sub tarsal
conjunctiva, in 6.4 % cases inferior fornix, in 1.8% cases superior fornix and
in 5.3% cases caruncle was involved. This is in contrast to study conducted by Reddy
et al where cornea was involved in 71.9% cases and in 28.03% cases conjunctiva
and fornices were involved. In another study11 conducted by Ozlem et
al cornea was involved in 72.6% cases. This difference may be due to
occupational variations12,13. Our study was conducted in a rural and
semi urban area where most of the population is involved in agriculture and
fields works. Corneal injuries most commonly occur due to metallic foreign bodies14.
This sort of injury is commonly seen in occupations associated with engineering
and industry15,16.
Ocular surface foreign bodies are found in
different locations in the eye. This emphasizes the importance of thorough eye
examination in case with history of foreign body in the eye.
In our study metallic particle was seen in
27.1% cases. This is less than the injury by metallic particles in other
studies. While in other studies similar percentage of metallic particle
injuries is reported17. In 25.6% cases part of insect body was
recovered from the eye. It may be due to driving practices of people. Most of
the people riding a bike and cycle do not use helmets and eye wear to protect
them from foreign bodies18. In 19.6% cases straw particles were found.
This is due to agricultural background of the region19.
In our study left eye was more commonly
injured in contrast to the study done by Reddy et al where right eye was more
commonly involved.
Ocular surface foreign bodies are found in
all parts of the ocular surface. More exposed parts like cornea and palpebral
conjunctiva are more prone to get such sort of injuries. Sub tarsal space gets
foreign bodies due to its anatomical configuration20,21. In our
study there was no statistically significant correlation of type of ocular
surface foreign bodies with their location of placement in the eye. Search of
literature could not reveal such type of correlation study. So we could not
compare our results with the work of others.
We did not include the
profession and occupation of the patients in our study. This is limitation of
our study. Moreover our study is limited to semi urban and rural area. Our
results may not be applicable for other settings.
CONCLUSION
Ocular surface foreign
bodies are common form of ocular trauma. More exposed parts of the ocular
surface receive majority of trauma due to superficial foreign bodies. Most
common aetiology of ocular surface injury was metallic particle and most common
location was cornea. No statistically significant correlation has been found
between the type of ocular surface foreign body with their location in the eye.
Author’s
Affiliation
MBBS, FCPS, Fellowship
Refractive and Cornea Surgery
Assistant Professor of
Ophthalmology,
Shahida Islam Medical College,
Lodhran.
Dr. Ahmad Zeeshan Jamil
MBBS, MCPS, FCPS, FRCS, FCPS
(VRO)
Assistant Professor of
Ophthalmology,
Sahiwal Medical College,
Sahiwal.
Role of
Authors
Dr. Muhammad Luqman Ali Bahoo
Concept and design of study and
interpretation of data
Dr. Ahmad Zeeshan Jamil
Drafting of the article and
critical revision for important intellectual content
REFERENCES
1.
Jan S, Khan S, Khan MT, et al. Ocular emergencies. J Coll Physicians Surg Pak. 2004; 14: 333-6.
2.
Guerra Garcia RA, Garcia D, Martinez FE et al. The Cuban ocular trauma registry. J Clin Exp Ophthalmol. 2013; 4
(2): 276.
3.
Negral AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998; 5:
143-69.
4.
Babar TF, Khan MN, Jan S, et al. Frequency and causes of bilateral ocular trauma.J Coll Physicians
Surg Pak. 2007; 17: 679-82.
5.
Khatry SK, Lewis AE, Schein OD, et al. The epidemiology of ocular trauma in rural Nepal. Br J
Ophthalmol. 2004; 88: 456-60.
6.
Injuries
to the eye. Sihota and Tandon,
editors. Parson’s disease of the eye. 20 Edition. New Delhi: Elsevier; 2007:
362-4.
7.
Abraham D, Vitale S, West S, et al. Epidemiology of eye injuries in rural Tanzania. Ophthamic
Epidemiol. 1999; 6: 85-94.
8.
Subba Reddy, P., Nirmala, K., Radhika, S., Ravi, S., Paul, C. Incidence of Ocular Surface Foreign Body and its Correlation with
Specific Occupation and Preventive Measures. Global journal for research
analyses, 2016; 5 (12): 56-8.
9.
Babar, T. F., Khan, M. T., Marwat, M. Z., Shah, S. A., Murad, Y.,
Khan, M. D. Patterns of ocular
trauma. J Coll Physicians Surg Pak. 2007; 17 (3): 148-153.
10.
Jahangir, T., Butt, N. H., Hamza, U., Tayyab, H., Jahangir, S. Patterns of Presentation and Factors Leading to Ocular Trauma.
Pak J Ophthalmol. 2011; 27 (2): 96-102.
11.
Güzel M, Erenler AK, Niyaz L, Baydın A. Management of traumatic eye injuries in the emergency department.
OA Emergency Medicine, 2014; 18 (1): 1-6.
12.
Fasih U, Shaikh A, Fehmi MS. Occupational ocular trauma (Causes management and prevention).
Pak J Ophthalmol. 2004; 20: 65-73.
13.
Mieler WF.
Ocular injuries: is it possible to further limit the occurrence rate? Arch
Ophthalmol. 2001; 119: 1712-3.
14.
Rama Krishnan T, Constantinous M, Jhanjiv, et al. corneal metallic foreign body injuries due to suboptimal ocular
protection. Arch Environ Occup Health, 2012; 67 (1): 48-50.
15.
Voon, L. W., See, J., & Wong, T. Y. The epidemiology of ocular trauma in Singapore: perspective from
the emergency service of a large tertiary hospital. Eye (Lond). 2001; 15 (Pt
1): 75-81.
16.
Gumus K, Karakucuk S, Mirza E. Corneal injury from a metallic foreign body: an occupational
hazard. Eye & contact lens, 2007; 33 (5): 259-60.
17.
Yigit O, Yuruktumen A, Arslan S. Foreign body traumas of the eye managed in an emergency
department of a single institution. Turkish journal of trauma & emergency
surgery, 2012; 18 (1): 75-9.
18.
Tahira MN, Hawortha N, Kinga M, Washingtona S, editors. Observations of Road Safety Behaviours and Practices of
Motorcycle Rickshaw Drivers in Lahore, Pakistan Australasian Road Safety
Conference, 2015; 14-16 October; Australia.
19.
Dass RI, Gohel DJ.
Ocular surface foreign body: its incidence and correlation with specific
occupation. GCSMC J Med Sci. 2013; 2 (2): 42-5.
20.
Alastair Denniston, P. M. Oxford Handbook of Ophthalmology, 2014; Oxford: OUP Oxford.
21.
Bowling, B. Kanski's
clinical ophthalmology a systematic approach, 2015; Sydnery: Saunders.